Monoclonal Gammopathy of Uncertain Significance (MGUS)
- < 3 gm/dL serum M protein (and)
- <10% clonal bone marrow plasma cells (and)
- Asymptomatic patients, no end organ damage (CRAB: hypercalcemia, renal insufficiency, anemia, bone lesions)
- No evidence of other B-cell lymphoproliferative disorder
MGUS is not considered “neoplastic” since most patients do not develop overt malignancy. A monoclonal M-protein is found in approximately 1 in 20 individuals after the age of 70. Similar to multiple myeloma, approximately 20% of patients will only have detectable free light chains.
The plasma cells are still clonal and patients have the following features
- 1% chance per year of progressing to multiple myeloma (0.3% for light chain MGUS).
- Non-IgM M-protein.
- 65% IgG
- 15% IgA
- 1% IgD
- 1% IgE
- 3% Biclonal
- Average bone marrow involvement of 3% plasma cells.
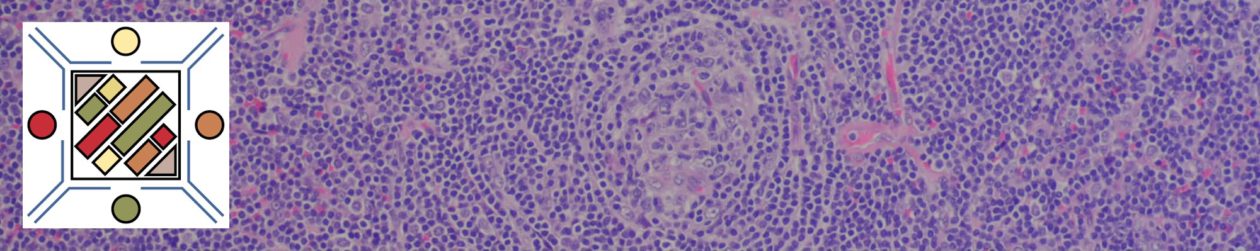
- Plasma cells have a mature appearance (cytoplasmic inclusions and nucleoli – occasionally).
- By flow cytometry these two populations can often be separated: (1) normal plasma cells CD19+/CD56- and (2) abnormal plasma cells CD19-/CD56+ or CD19-/CD56- (other aberrant antigen expression may also be present).
- From a molecular prospective, there are no definite differentiating factors between MGUS and multiple myeloma (although this may change).
- Free Light Chain MGUS
- Urine light chain excretion <0.5 g/24 hours
- <10% plasma cells in bone marrow
- No end-organ damage
IgM MGUS is considered as a precursor to lymphplasmacytic lymphoma (LPL) and/or Waldenstrom and is separate from Non-IgM MGUS (IgG, IgA), which is a precursor to multiple myeloma.
References
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015. pp. 599-601.
WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. SH Swerdlow, et al. International Agency for Research on Cancer. Lyon, 2008. pp. 200-213
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127: 2375–2390. doi:10.1182/blood-2016-01-643569