There have been several attempts at subtype classification with varying acceptance based on morphology, immunophenotype, and molecular characteristics. Gene expression profiling (GEP) studies have demonstrated distinct molecular subtypes (germinal center B-cell-like vs. activated B-cell-like). GEP is not routinely available, and immunohistochemical surrogate markers have been employed to substitute with an acceptable sensitivity rate. The most commonly used IHC surrogate is the Hans’ algorithm.
DLBCL cases with the “double/triple” hit, which consists of a MYC translocation combined with a BCL-2 and/or BCL6 translocation(s), is associated with a very aggressive course and poor prognosis. These cases are usually considered for Burkitt lymphoma type chemotherapy regimens, and have been reclassified as a high grade lymphoma (like Burkitt lymphoma) in the 2016 WHO revision.
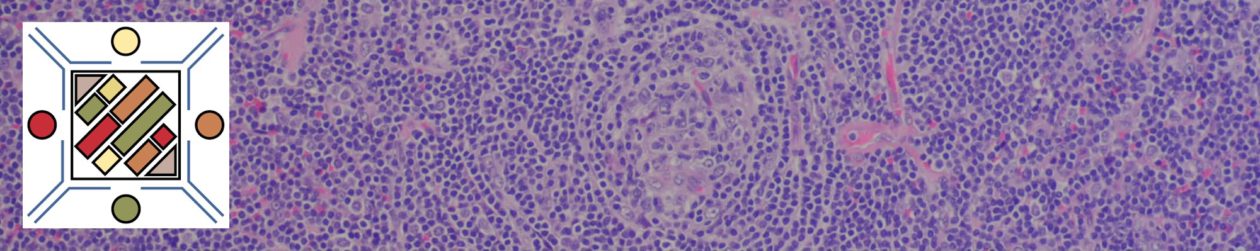
DLBCL, NOS Morphologic Variants
- Anaplastic – large cells with pleomorphic/bizzare nuclei. May be difficult to differentiate from ALCL, Hodgkin lymphoma, or carcinoma.
- Immunoblastic – >90% of the cells have an immunoblastic morphology with a prominent single centrally located nucleoli and basophilic cytoplasm (plasmacytoid differentiation may also be present)
- Centroblastic – medium to large cells with oval to round nuclei, 2-4 nucleoli, vesicular nuclei. Can be pure centrocblasts or mixed with immunoblastic cells.
DLBCL, NOS Molecular Subtypes
- Germinal Center B-cell-like (GCB)
- Activated B-cell-like (ABC)
DLBCL, NOS Immunophenotypic Subtypes
- CD5+ DLBCL
- Germinal Center B-Cell-Like (GCB)
- Non-Germinal Center B-Cell-Like (non-GCB)
Other Recognized Diffuse Large B-Cell Lymphoma Subtypes
- T-Cell/Histiocyte Rich Large B-Cell Lymphoma
- Primary DLBCL of the CNS
- Primary Cutaneous DLBCL, Leg Type
- EBV+ DLBCL of the Elderly
Immunophenotype
- Positive for B-Cell markers: CD19, CD20, CD22, and CD79a
- CD5 – positive in ~5% of cases. Important to exclude a blasted variant of mantle cell lymphoma or transformation from mantle cell lymphoma. May need to use cyclin D1 (bcl-1) or FISH for t(11;14). CD5+ cases may be associated with more aggressive course, CNS involvement, and bone marrow involvement. Intravascular DLBCL is a separate subtype and often CD5+.
- CD10 – positive in 30-60% of cases, and according to the Hans criteria defines the germinal center B-cell-like group, which is associated with a better prognosis.
- Bcl-6 – positive in 60-90% of cases and is a marker of germinal center nuclei. Also used in the Hans criteria algorithm to classify as GCB or non-GCB phenotypes.
- MUM-1/IRF4 – is a marker of post-germinal center differentiation and is expressed in 35-65% of cases. Also used in the Hans criteria (>30% expression is used as a cut off for positive in the Hans criteria).
- Bcl-2 – thought by some to be an independent adverse prognostic marker. However, this finding appears to be dependent upon the treatment situation, and in the setting of rituximab therapy may have opposite finding of being a good prognostic marker (Chan).
- CD30 – expressed in approximately 14% of DLBCL cases. In the absence of EBV+, CD30 expression is a good prognostic marker. This marker may also have relevance in refractory disease with new monoclonal antibody drugs to CD30 (brentuximab vedotin).
- PD-L1 – increased expression has been found in ~20% of DLBCL, NOS (particularly non-GCB phenotype), and raises the possibility for a therapeutic role of PD-L1 inhibitors (under investigation).
Chromosomal abnormalities
- Bcl-6 (3q27) translocations – Up to 30% of cases
- Bcl-2 t(14;18) translocations – 10-20%, up to 30%
- MYC translocations – ~5%, up to 10%
Molecular profiles
- Geminal Center B-Cell-Like (GCB) – relatively better prognosis/survival; most will substitute IHC markers (e.g. Hans classifier) as a surrogate.
- Activated B-Cell-Like (ABC) – relatively worse prognosis; most will substitute IHC markers (e.g. Hans classifier) as a surrogate. ABC/non-GCB vs. GCB classification will often determine treatment plans, and now appears to have prognostic and predictive value.
Other B-Cell Lymphomas with large cells not cover under this heading:
- Primary Effusion Lymphoma
- Primary Mediastinal (Thymic) Large B-Cell Lymphoma
- Intravascular Large B-Cell Lymphoma
- DLBCL associated with Chronic Inflammation
- Large B-Cell Lymphoma arising in HHV-8-Associated Multicentric Cattleman Disease
- ALK+ Large B-Cell Lymphoma
- Lymphomatous Granulomatosis
- Plasmabalstic Lymphoma
2016 WHO Revision Changes for DLBCL
- ABC/non-GCB vs. GCB characterization is required part of DLBCL classification
- BCL-2 & MYC dual expression by IHC considered as “double expresser” lymphoma, which has a more aggressive course (not to be confused with the “double/triple” hit lymphoma.