Plasma Cell myeloma (PCM) is a disorder of monoclonal plasma cells, which is almost always associated with a monoclonal immunoglobulin protein in the serum and/or urine along with end organ damage (e.g. lytic bone lesions, renal failure, etc.).
Plasma cell myeloma is defined as the combination of a monoclonal proteins (M component) with clonal bone marrow plasma cells and end organ damage (CRAB: hypercalcemia, renal insufficiency, anemia, bone lesions – not exclusive, other manifestations of end organ damage include amyloidosis, hyper-viscosity, recurrent infections, etc.)
WHO PCM Diagnostic Criteria
- ≥10% monoclonal plasma cells (or) biopsy proven plasmacytoma (and)
- ≥1 myeloma defining event
- End-organ damage
- Hypercalcemia (>1 mg/dL above upper limit of normal or >11 mg/dL)
- Renal insufficiency
- Creatinine clearance <40 mL/minute (or)
- Serum creatinine > 2 mg/dL
- Anemia
- Hgb >2 g/dL below lower limit of normal
- Hgb <10 g/dL
- Bone lesion(s) – ≥1 lytic lesion (skeletal survey, CT, or CT/PET)
- Biomarker of Malignancy
- ≥60% monoclonal plasma cells
- ≥100 serum free light chain ratio (involved-to-uninvolved)
- >1 focal lesion on MRI
- End-organ damage
Common findings:
- Lytic bone lesions
- Immune dysregulation
- Renal insufficiency
- Monoclonal plasma cells (>3 gm/dL serum Ig and/or >6 mg/dL of urine Bence-Hones protein)
- Hypercalcemia
Multiple Myeloma (Symptomatic Plasma Cell Myeloma)
- Usually >3 gm/dL serum M protein and/or >6 g/dL urine Bence-Jones protein
- 60-70% of patients have both
- 20% only free light chains
- Non-Secretory Myeloma Variant: ~1-3% of Multiple Myeloma cases
- Clonal bone marrow plasma cells
- Symptomatic patient / evidence of end organ damage (CRAB: hypercalcemia, renal insufficiency, anemia, bone lesions)
Molecular genetics
Plasma cell myeloma (PCM) shows significant molecular heterogeneity. Translocations involving the immunoglobulin heavy chain (IgH) are common and often include partner genes of cyclin D1 on 14q13 and cyclin D3 on 6p21 (translocation with cyclin D1 is associated with a good outcome). Deletion of the TP53 tumor suppressor gene on chromosome 17 is associated with a poor prognosis (deletions of 13q and t(4;14) are also associated with a more aggressive course). Many other abnormalities and translocations have been identified but are beyond the brevity of this discussion.
Immunophenotype
Plasma cells express CD138 (sydecan-1), and a subset of cases express CD56, which is not present on normal plasma cells. CD56 can be helpful in identifying neoplastic plasma cells.
- CD138 – Positive
- CD56 – 75-80% Positive
- CD20 – 10-20% Positive
- CD117 – 20-35% Positive
Plasma cell leukemia is defined as >2 x 10^9/L or >20% clonal plasma cells in the peripheral blood.
Plasmacytoma
Smoldering (Asymptomatic) Myeloma
Monoclonal Gammopathy of Uncertain Significance (MGUS) – Non-IgM
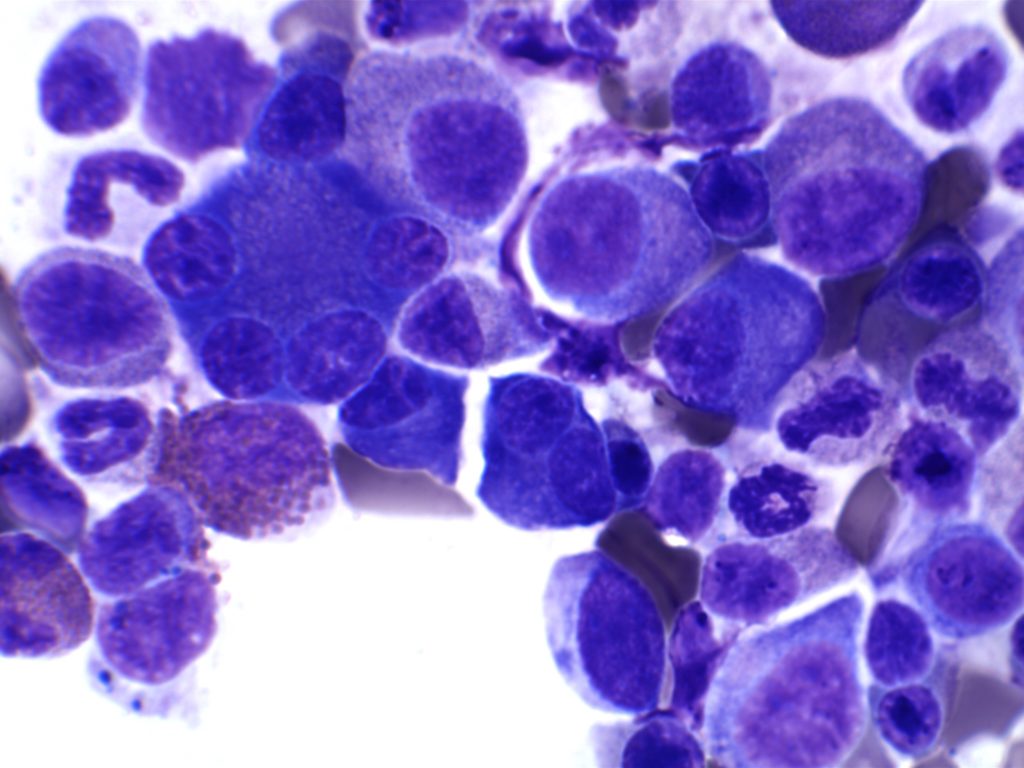
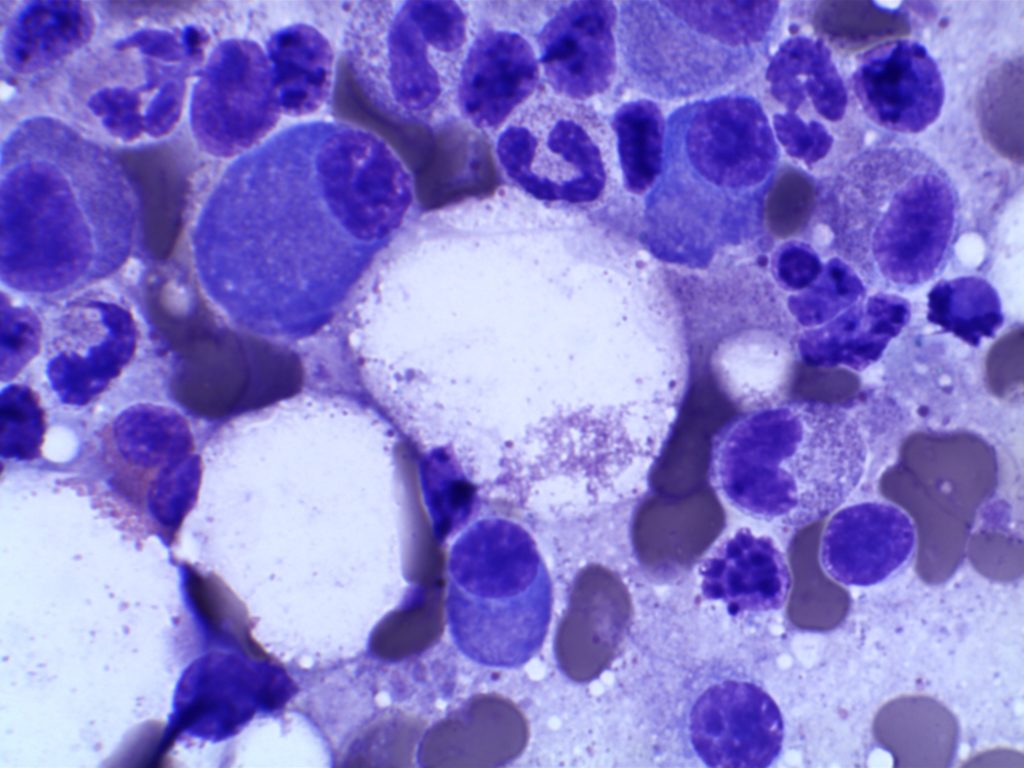
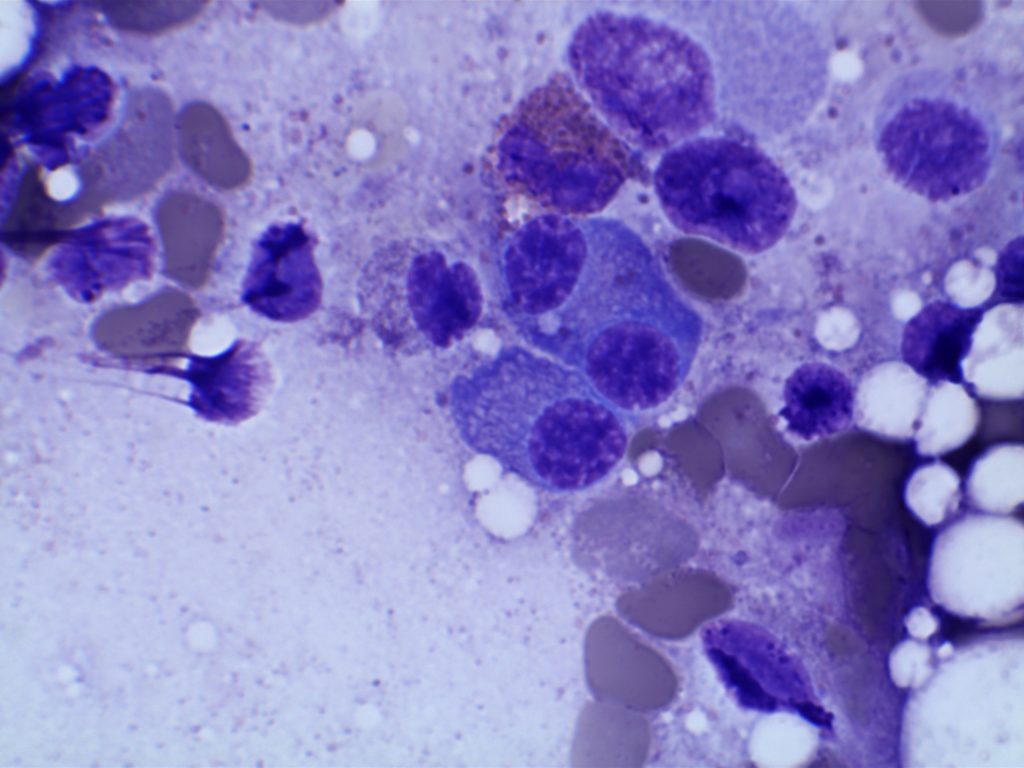
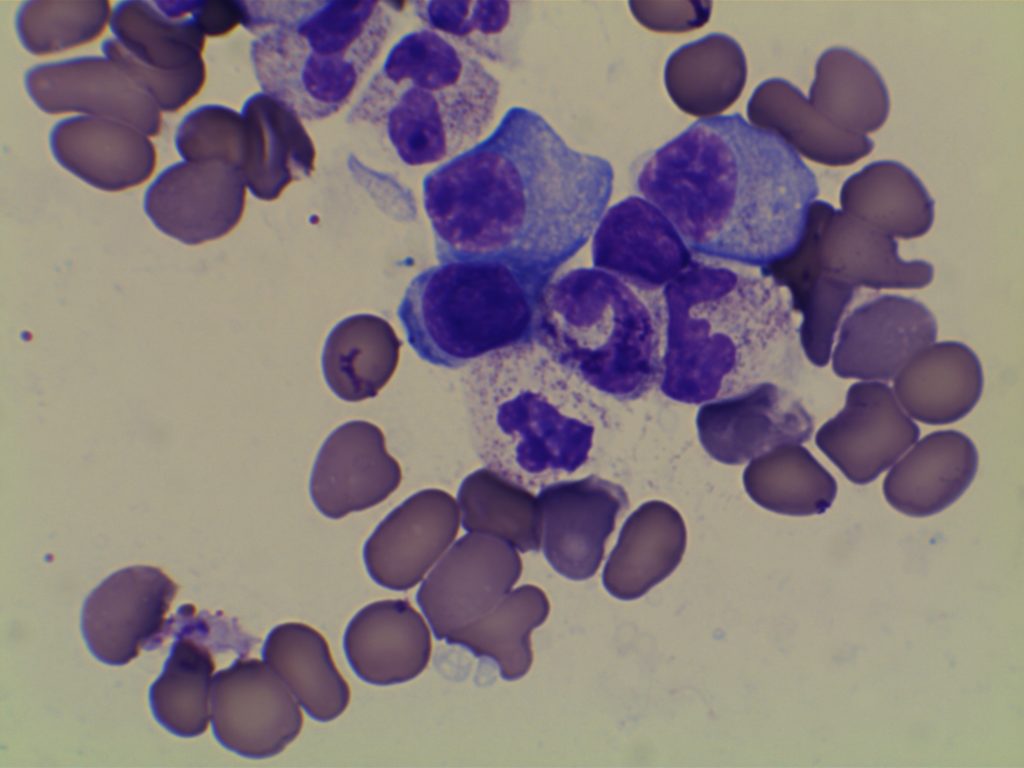
Photomicrographs
References
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015. pp. 599-601.
WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. SH Swerdlow, et al. International Agency for Research on Cancer. Lyon, 2008. pp. 200-213
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127: 2375–2390. doi:10.1182/blood-2016-01-643569